As monkeypox (now officially referred to as mpox) continues to circulate globally, healthcare providers need to be prepared with the best tools and practices for accurate testing.
Early detection and effective testing are crucial for isolating cases, preventing outbreaks, and managing public health.
In this guide, we’ll explore how healthcare professionals can collect specimens for monkeypox testing, discuss the tools required for swabbing, and share expert tips for ensuring the integrity of each sample. Whether you're navigating a busy clinic or a lab, understanding the swabbing process is essential to protecting your patients and the community.
What is Mpox (a.k.a. Monkeypox)?
Mpox (Monkeypox) is a viral infection caused by the monkeypox virus, part of the Orthopoxvirus family, which includes the more well-known smallpox virus. Though less severe than smallpox, monkeypox can still cause significant illness, particularly in vulnerable populations. The infection is characterized by flu-like symptoms followed by a rash that progresses through several stages, eventually forming scabs that fall off. Understanding how to identify and test for this virus is crucial for healthcare providers, as early detection plays a vital role in controlling its spread.

How monkeypox is spread
Anyone can catch monkeypox if they have close contact with someone infected with the virus. Because Mpox is a zoonotic disease, the CDC explains that while the monkeypox virus is not easily spread, it can be passed from an infected animal, infected person, or materials contaminated with the virus. The most common animals that have been infected by Monkeypox are African squirrels and other rodents. This is coupled with the rise in Avian Flu in recent years, showcasing the increased risk of zoonotic diseases to humans.
The virus spreads through direct contact with an infected person’s body fluids or lesions or materials that have touched body fluids or lesions, such as clothing or linens. It also can be spread through respiratory secretions during prolonged, face-to-face contact.
Individuals who believe they have come into contact with someone infected by the monkeypox virus should pursue testing. Healthcare providers that suspect a case of monkeypox should contact their county health department to obtain monkeypox virus-specific real-time polymerase chain reaction (PCR) testing and to report the occurrence.
Common symptoms associated with Mpox (Monkeypox)
According to the Centers for Disease Control and Prevention (CDC), Monkeypox presents with a variety of symptoms that can range from mild to severe. Typically, the illness begins with flu-like symptoms, followed by the development of a distinctive rash.
Here are the most common signs and symptoms of monkeypox:
-
Fever: One of the earliest symptoms of monkeypox is a high fever, which may last for several days.
-
Headache: Patients often experience persistent headaches alongside other flu-like symptoms.
-
Muscle Aches and Backache: General muscle soreness, including back pain, is common during the early stages of infection.
-
Swollen Lymph Nodes: Unlike smallpox, which is closely related to monkeypox, this virus often causes swelling of the lymph nodes (lymphadenopathy). This is a distinguishing feature of monkeypox, helping healthcare providers differentiate it from other poxvirus infections.
-
Chills and Exhaustion: Patients may feel extreme fatigue and experience chills, as their bodies fight the infection.
-
Lesions/Rash: The most characteristic symptom of monkeypox is a rash that appears 1-3 days after the onset of fever. The rash often starts on the face and spreads to other parts of the body, including the hands, feet, chest, and genitals. The lesions typically progress through several stages, starting as macules (flat spots), then evolving into papules (raised bumps), vesicles (fluid-filled blisters), pustules (pus-filled lesions), and eventually scabs that fall off.

Some patients may only experience a rash without the flu-like symptoms, while others may notice the rash appearing first. The severity of symptoms can vary, but the presence of lesions on the skin is a telltale sign that healthcare providers look for when diagnosing monkeypox.
You’ll note that many of these symptoms are very similar to other seasonal illnesses, making it more challenging to diagnose. The lesions are the key piece of the puzzle to look out for.
Note: If healthcare providers suspect a possible case of monkeypox, immediately contact your county health department. Local county health departments can help providers obtain monkeypox virus-specific real-time polymerase chain reaction (PCR) testing.
The history of monkeypox
Monkeypox was first identified in 1958 during an outbreak in an animal facility in Copenhagen. However, the virus gained global attention with recent outbreaks in non-endemic regions, including the U.S. and Europe. As the virus spreads through close contact and respiratory droplets, it poses a significant risk, especially during outbreaks in densely populated areas.
Why is Mpox (Monkeypox) a global health threat
Monkeypox has recently emerged as a global public health concern due to outbreaks in non-endemic regions like the United States and Europe, where it was previously rare.
Mpox (Monkeypox) in the United States
While there continue to be numerous cases of Monkeypox in African countries, with particular concentration in the Democratic Republic of the Congo (DRC), this is not the case in the United States. However, U.S. public health officials, along with the CDC and the Department of Health and Human Services (HHS), have ramped up preparation efforts to control the spread of monkeypox in the instance that the current status changes. If someone is diagnosed, testing and isolation remain critical components of managing outbreaks and preventing further transmission.
Why testing and swabbing for monkeypox is important
While the fatality rate for Monkeypox is low (0.1-1% of all cases) and most people will recover without healthcare intervention, timely and accurate testing is crucial to containing the virus. Early detection allows healthcare providers to isolate patients and initiate appropriate treatment. Testing is also essential for public health authorities, enabling them to trace outbreaks, monitor trends, and implement necessary measures to prevent further spread.
Testing for monkeypox is performed using real-time polymerase chain reaction (PCR) testing on lesion samples. Given the similarity in symptoms between monkeypox and other viral infections such as chickenpox, accurate specimen collection is vital for correct diagnosis.
It’s important to note that there is no approved treatment for monkeypox to-date.
Download our step-by-step printable Mpox testing guide below:
Challenges in testing for Mpox (Monkeypox)
One of the major challenges healthcare providers face in testing for monkeypox is distinguishing it from other diseases that cause similar symptoms.
According to the National Library of Medicine, chickenpox, smallpox, varicella, primary and secondary syphilis, acute retroviral syndrome, genital herpes simplex virus, and certain skin rashes can present similarly, making it important to collect specimens accurately.
Additionally, not all facilities are fully equipped to handle mpox testing, which underscores the importance of knowing the proper collection techniques and working with state health labs.
How providers are handling Mpox (Monkeypox) testing
As monkeypox cases continue to spread globally, healthcare providers and laboratories have ramped up their testing capabilities to meet the demand. Many hospitals and clinics have implemented protocols to identify potential monkeypox cases quickly and efficiently, ensuring timely diagnosis and isolation to prevent further spread.
State public health laboratories, alongside the CDC, have played a crucial role in building testing capacity. Public health agencies across the U.S. have established networks to process monkeypox tests, ensuring that confirmed cases are reported promptly.
The CDC continues to work with state and local health departments to monitor testing volumes and ensure they meet the needs of the public.
When handling suspected monkeypox cases, healthcare professionals are advised to wear appropriate personal protective equipment (PPE) such as gowns, gloves, eye protection, and N95 respirators to minimize the risk of exposure. The CDC also provides specific protocols for collecting, storing, and transporting specimens for monkeypox testing to ensure that samples are handled safely and that accurate results are obtained.
How to swab for Mpox (Monkeypox)
Accurate specimen collection is the cornerstone of effective monkeypox testing. Here’s a detailed guide on how healthcare providers can collect samples for testing for patients with lesions:
Step 1: Prepare your swabs
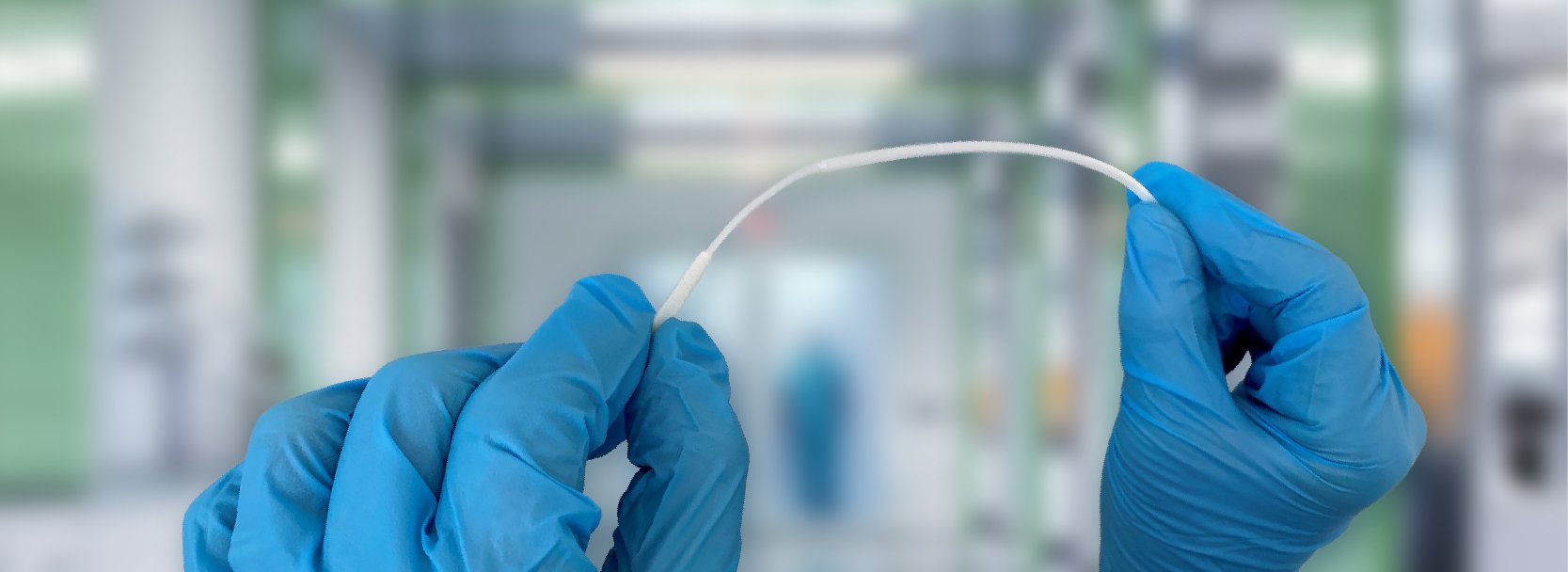
The first step in collecting a specimen for monkeypox testing is choosing the correct swab. The CDC recommends using sterile, dry swabs made from materials like nylon or polyester. These swabs must have shafts made of plastic or slender metal or wire, as cotton swabs are not suitable. Cotton can interfere with the collection and release of the sample, compromising the integrity of the results.
For optimal collection and diagnostic accuracy, Puritan’s HydraFlock® and PurFlock Ultra® swabs are excellent choices. These swabs feature multi-length polyester fibers that assure efficient specimen collection and release, making them ideal for monkeypox testing.
Step 2: Collect the sample
To collect a specimen for testing:
-
Swab at least two different lesions from different parts of the body.
-
Swabbing multiple lesions helps ensure enough viral material is collected for accurate testing.
-
If a lesion appears dry or crusty, it is recommended to moisten the swab with sterile saline to improve collection.
-
Vigorously swab or brush the lesion with a sterile swab, ensuring enough material is gathered for both preliminary and confirmatory testing.
It is essential to wear personal protective equipment (PPE), including gloves, gowns, and N95 masks, during the collection process to protect against contamination and the spread of the virus.
Step 3: Store the sample
After collection, each swab should be placed into its own sterile, dry container. Avoid adding any transport media or liquid to the container, as it can interfere with PCR testing. Proper storage of the sample is key to preserving its integrity for testing.
Step 4: Label the sample
Clearly label each sample with the patient’s name, date of birth, collection date, and collection site. Proper labeling is crucial for accurate record-keeping and ensures that the sample can be traced back to the correct patient throughout the testing process.
Step 5: Refrigerate or freeze the sample
To preserve the sample’s viability, it is recommended to refrigerate the specimen within one hour of collection at a temperature between 2–8°C. Samples can be stored refrigerated for up to 7 days. If freezing is required, store the sample at -20°C or lower, which allows for storage of up to 60 days.
Step 6: Send the sample for lab testing
Once properly labeled and stored, the sample should be sent to the appropriate public health laboratory for testing. Ensure the sample is shipped according to regulatory guidelines to prevent any degradation during transit. The first swab is usually tested at the state lab for a presumptive diagnosis. If positive, the second swab may be sent to the CDC for confirmatory testing.
If a patient doesn’t have lesions…
The UK Health Security Agency recommends, “For high-risk contacts of a confirmed case who have developed systemic symptoms but does not have a rash or lesions for sampling, you should take a throat swab in viral transport media.” For more information on how to collect a throat swab specimen, download our free infographic here.
Note that even if the throat swab is negative, continue to monitor and isolate the individual in accordance with guidance, reassessing and testing if further symptoms develop.
Want a printable guide for your clinic? Download our step-by-step Mpox testing guide here:
Two key tips for accurate Monkeypox testing
To ensure you get the best quality sample possible and receive accurate test results, we recommend:
1. Avoiding cross-contamination
To ensure accurate monkeypox (mpox) test results, avoiding cross-contamination is essential. Healthcare providers should wear full personal protective equipment (PPE), including gloves, gowns, eye protection, and an N95 respirator, when handling patients and specimens. This minimizes the risk of contaminating the sample or exposing healthcare staff to the virus.
When collecting specimens, it's crucial to test in a clean setting, free from any contamination. Use a separate, sterile swab for each lesion, and avoid touching surfaces or other lesions with the swab to ensure the sample is uncontaminated. Proper swabbing technique is critical to collecting a reliable sample for testing.
2. Adhering to proper storage and handling
Once the sample is collected, it is important to store and transport it correctly to maintain its integrity. Follow the CDC guidelines to ensure the specimen remains viable for testing.
Samples should be refrigerated within one hour of collection, at a temperature between 2°C and 8°C, and can be stored for up to seven days. For longer storage, freeze the sample at -20°C or lower, where it can remain viable for up to 60 days. Always place the swab in a sterile, dry container and avoid using transport media or any liquids, as they can affect test accuracy.
Proper tools & supplies for accurate Monkeypox swabbing
Accurate monkeypox testing requires using the right diagnostic tools to ensure proper specimen collection, storage, and transport. Selecting the right swabs and other materials is crucial to maintain sample integrity and support accurate laboratory analysis.
What swabs to use for Mpox (Monkeypox) testing
When collecting specimens for mpox testing, it’s recommended to use sterile, synthetic fiber-tipped swabs, with sturdy handles. For optimal specimen collection, we recommend using the following swab types:
Puritan 6" Sterile Standard Polyester Swab w/Polystyrene Handle (SKU # 25-806 1PD)
Puritan 6" Sterile Standard Polyester Swab w/Solid Polystyrene Handle (SKU # 25-806 1PD SOLID)
Puritan 6" Sterile Standard Polyester Plastic Handle Swab & Tube (SKU # 25-806 1PD BT)
Puritan UniTranz-RT 3ml Filled Vial w/ 6" Sterile Standard Polyester Swab (SKU # UT-361)
Puritan UniTranz-RT 3ml Filled Vial w/2 Sterile Standard Polyester Swabs (SKU # UT-362)
Puritan UniTranz-RT 3ml Universal Transport Solution - Vial Only (SKU # UT-300)
Transport tubes
Dry transport tubes play a critical role in maintaining the integrity of the specimen during transport to the testing laboratory. The CDC recommends using plastic tubes instead of glass to prevent accidental breakage. Puritan’s dry transport system tubes are made from virgin polypropylene resin, creating a sterile and safe environment for the swab during transit.
Each transport tube is designed with a precision-fitted, injection-molded cap that eliminates the risk of contamination. Proper labeling on the tube is essential, displaying product expiration dates and providing space for patient identification and collection details. In some cases, the label acts as a seal between tube and cap, assuring the sterility of the swab inside.
Viral transport medium
While the use of viral or universal transport medium is not always required for monkeypox testing, it can enhance the accuracy of specimen collection by preserving the sample during storage and transport. Viral transport mediums help maintain a balanced buffer solution, ensuring a neutral pH, while also incorporating antimicrobial agents, protein sources, and sucrose to preserve the sample's integrity.
Puritan offers various configurations of universal transport media and molecular preservatives, such as the UniTranz-RT and PurSafe solutions, which are ideal for use with monkeypox specimens.
Resources: improving your swabbing technique for Mpox (Monkeypox)
To learn more about monkeypox, as well as testing and treating the disease, consider the following resources:
To learn more about the types of diagnostic tools available for accurate testing, contact the Puritan team.