Sexually Transmitted Infections (STIs) are an important issue in our country, showcasing the need for heightened STI awareness now more than ever. In 2023, according to the Centers for Disease Control and Prevention (CDC), there were over 2.4 million reported STI cases in the United States alone.

While there is positive news that rates have technically declined, the rate of infection is still quite high and the need for vigilance remains a top priority for people who engage in sexual activity.
Join us as we dive deeper into the STI epidemic in the United States, sharing why STI awareness is critical for whole person health and what we can do to test for and prevent STIs.
Why is STI Awareness Important?
The CDC points out that STIs do not always cause symptoms. This means that diagnosis is critical for preventing transmission. If left untreated, STIs can lead to issues ranging from difficulty getting pregnant to pelvic inflammatory disease, damage to the brain or nervous system, and other serious health issues.
This increased risk is precisely why STI awareness and screening is critical. Healthcare providers seeking to build this awareness may begin by explaining the ease and benefits of STI testing, and when it may be possible to conduct a test using today’s STI swabs designed for minimally invasive self-collection.
How to Improve STI Awareness
Improving STI awareness starts with open, accurate conversations—both in and out of the clinic. Healthcare professionals play a key role in normalizing testing, debunking myths, and promoting safer sexual practices. Patient education materials, visual guides, and approachable language can make a huge difference in how information is received and retained.
Clinics and health organizations can also improve outreach through community events, social media campaigns, and partnerships with local schools or universities. The more accessible and judgment-free the conversation, the more likely individuals are to seek testing and treatment when needed.
What and When is STI Awareness Month?
STI Awareness Month is observed every April in the United States. This month-long initiative, led by the CDC and other public health agencies, focuses on increasing awareness of sexually transmitted infections and encouraging preventative behaviors like regular testing, safer sex practices, and open communication. It's also a time to highlight the importance of reducing stigma and ensuring equal access to testing and treatment services.
Is There a Difference Between an STI and STD?
Yes, and it’s more than just semantics.
STI stands for sexually transmitted infection, while STD refers to sexually transmitted disease. The term "STI" is now more widely used in healthcare because it reflects the reality that many infections don’t cause immediate symptoms or progress into diseases.
For instance, someone can carry an infection like chlamydia without showing symptoms, making “infection” a more accurate term in many cases. Using "STI" also helps reduce stigma and encourages more people to seek regular screening.
What are the Incurable Sexually Transmitted Infections?
When it comes to sexual health, incurable sexually transmitted infections present unique challenges for both patients and providers. These infections cannot be completely eradicated from the body, but with proper management, individuals can still lead healthy lives and reduce the risk of transmission.
Common incurable STIs include:
-
Herpes Simplex Virus (HSV) – Causes genital or oral herpes. While there’s no cure, antiviral medications can reduce symptoms and outbreaks.
-
Human Immunodeficiency Virus (HIV) – Attacks the immune system over time. Modern antiretroviral therapy (ART) can suppress the virus to undetectable levels, preventing transmission and preserving health.
-
Human Papillomavirus (HPV) – Some high-risk strains of HPV can lead to cancer. There’s no treatment for the virus itself, but regular screenings and the HPV vaccine can prevent complications.
-
Hepatitis B (HBV) – Although a vaccine exists, chronic HBV infections can occur. Antiviral treatments can help manage viral load and protect liver function.
Awareness, early detection, and consistent care are key to managing incurable sexually transmitted infections.
Testing and vaccination play vital roles in prevention, and patient education helps reduce stigma, improve treatment adherence, and encourage safer practices.
Which leads us to…
What is a Standard STI Test?
A standard STI test typically includes screening for the most common and high-risk infections: chlamydia, gonorrhea, syphilis, HIV, and often trichomoniasis. Depending on the patient’s sexual history and risk factors, providers may also test for hepatitis B/C, herpes, and HPV. Tests can involve a combination of swabs (vaginal, urethral, throat, or rectal), urine samples, and blood draws.
Clinics may use tools like the Hologic® Aptima Combo 2 Test, which detects chlamydia and gonorrhea from a single swab, for efficient and accurate diagnosis.
Since it’s our specialty, let’s dive into a bit more about STI swabs.
What is an STI Swab?
While syphilis and some other STIs must be confirmed by a blood test, gonorrhea and chlamydia can be diagnosed by collecting a sample from the genitals, throat, or rectum using an STI swab.
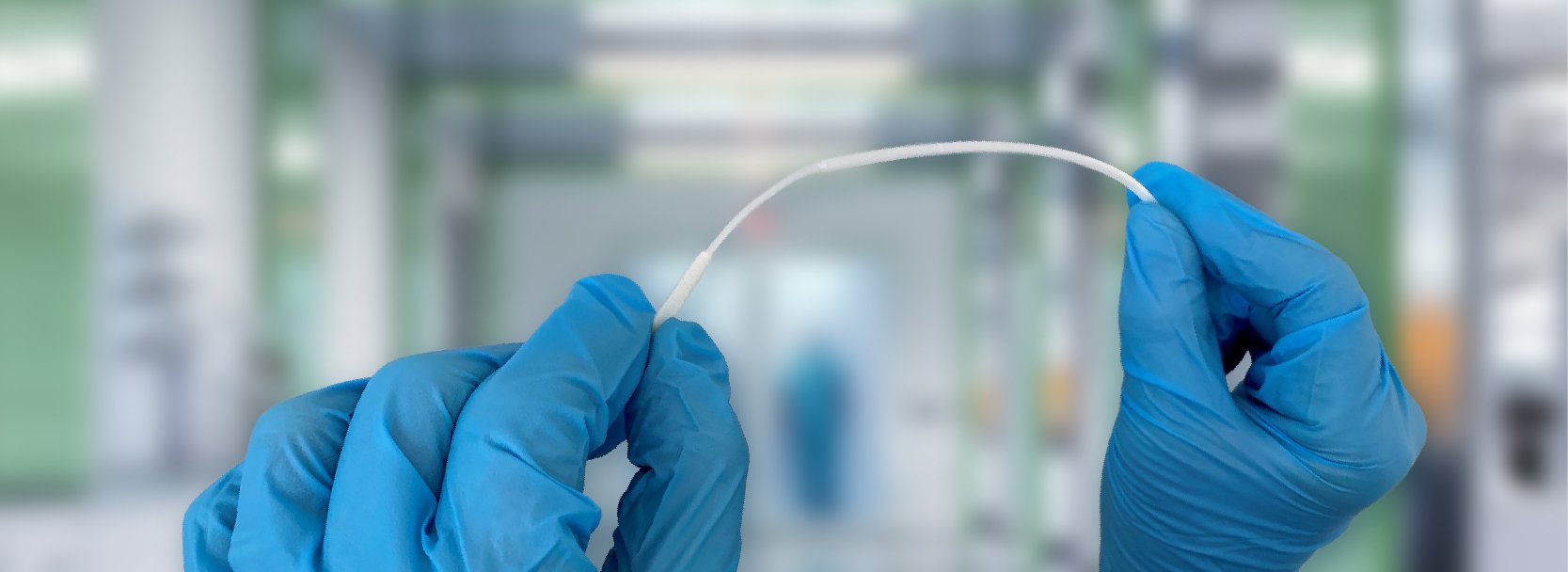
An STI swab is specially designed to collect a sample without irritating the patient or contamination of the sample. This swab can be used in conjunction with a transport kit or to carry the collected specimen directly to the lab for assay. A number of options are available for these swab tests. An endocervical sample, collected from the area around the opening of the uterus, is a preferred site for specimen collection from females. A urethral sample, collected from the urethra, is a preferred collection site in men or in women with no cervix.
In some instances, clinicians allow for self-collection of samples through a penile swab test or vaginal swab test. Self-collected specimens can often be tested using Nucleic Acid Amplification Tests (NAATs), which have proven reliable for testing a number of STIs.
What is the Best Material for an STI Swab?
For diagnostic specimen collection, providers should insert a collection swab with a synthetic tip on a synthetic handle. However, different tests may benefit from using different swab types.
For a vaginal swab test, a spun fiber swab such as the 25-806 1PR rayon-tipped swab (pictured below) or 25-806 1PD polyester-tipped swab will collect an ample specimen with minimal discomfort. For endocervical specimen collection, providers may consider a flock swab, such as the 25-3306-U PurFlock Ultra.
For male specimen collection, clinicians may consider the 25-800 D 50 polyester mini-tip (pictured below) on an aluminum handle or the 25-800 1PD ALUM 50, which features a polyester mini-tip on aluminum wire that is sleeved with a plastic handle for ease of use. Practitioners might also opt for a flock mini-tip swab such as the 25-3317-U.
To minimize the reporting of a false result, the CDC recommends confirmatory testing of positive test results. This means a second test may be recommended, and clinicians should consider this need in managing their inventory levels.
What is a Penile STI Swab Test?
Penile meatal swabs allow for self-collection of samples, as opposed to more invasive clinician-collected urethral swab testing. A penile swab test collects a sample outside the opening of the penis, and does not require that the swab be inserted into the penis. This form of sampling may be used to test for M. genitalium, chlamydia, gonorrhea and human papillomavirus (HPV), among other pathogens.
What is a Vaginal STI Swab Test?
Vaginal swabs allow for the self-collection of samples for a number of STIs. These minimally invasive tests provide similar sensitivity to clinician-collected swabs, according to CDC. Vaginal swab tests may be used to detect the presence of chlamydia, gonorrhea, C. trachomatis, M. genitalium, bacterial vaginosis, and Trichomoniasis, among other STIs.
Resources for Doing a Standard STI Swab Test
Clinicians should provide guidance to patients prior to self-collection of samples using an STI swab kit. A proper approach to sample collection is necessary to ensure an ample amount of specimen is gathered without risk of contamination.
Puritan provides resources that clinicians can use to help patients in self-sampling for vaginal collection or penile collection.
Why Use Puritan for Your STI Swab Needs
Because all of our swabs are made right here in the U.S.A., Puritan Medical Products delivers the highest quality swabs when you need them. If you’re ready to place an order, or simply want to determine the best swab for your specific needs, we encourage you to reach out to the Puritan sales team today.