Testing for Enterovirus (EV-D68) has gained importance due to its potential to cause respiratory illnesses, particularly in children and individuals with asthma. Yet, for many healthcare providers, testing for enterovirus strains remains challenging.
Understanding how to test for enteroviruses, what methods are available, and how to collect and submit specimens accurately is crucial for early detection and treatment. In this guide, we’ll break down the key facts about this illusive virus, when to test, and how to ensure your specimen collection process is precise.
What is Enterovirus?
First discovered in California in 1962, Enteroviruses are a large family of viruses that cause a wide range of illnesses, from mild cold-like symptoms to severe respiratory and neurological conditions. Enteroviruses are primarily transmitted through respiratory secretions, close personal contact, or contact with contaminated surfaces.
They are highly contagious and can spread rapidly, particularly in places like schools and childcare centers.
Overview of the Enteroviruses family
The enterovirus family is a large and diverse group of viruses that includes over 100 strains, responsible for a wide range of illnesses. These viruses are part of the Picornaviridae family and are classified into four main species: Enterovirus A, B, C, and D.
Some of the most notable strains within the enterovirus family include:
Enterovirus D68 (EV-D68)
This strain is known for causing respiratory illnesses, particularly in children. It has been associated with outbreaks of severe respiratory illness, sometimes leading to serious complications such as paralysis.
Coxsackieviruses
These viruses are divided into Group A and Group B. Group A coxsackieviruses are typically associated with hand, foot, and mouth disease, while Group B coxsackieviruses can cause more severe conditions like viral meningitis, myocarditis (inflammation of the heart muscle), and pericarditis (inflammation of the lining of the heart).
Poliovirus
Perhaps the most well-known enterovirus, poliovirus, is the cause of polio, a crippling disease that can lead to paralysis and death. Thanks to widespread vaccination efforts, polio has been largely eradicated in many parts of the world, though it remains endemic in a few regions.
Other strains in the enterovirus family can cause illnesses ranging from mild cold-like symptoms to severe neurological conditions, making it essential to accurately identify and test for these viruses, especially during outbreaks. Understanding the wide-ranging impact of enteroviruses can help healthcare providers respond effectively and take appropriate preventive measures.
Symptoms of Enterovirus
Enterovirus presents with a wide spectrum of symptoms that range from mild, flu-like signs to more severe respiratory issues. While many infected individuals may experience mild discomfort, the virus can pose a significant threat to high-risk populations, particularly children, individuals with asthma, and those with weakened immune systems.
Mild Symptoms
-
Runny nose: One of the earliest and most common symptoms of EV-D68, often mistaken for a cold or seasonal allergies.
-
Sneezing: Frequent sneezing, which contributes to the easy spread of the virus, especially in crowded environments like schools.
-
Cough: A persistent cough, which can vary from mild to severe, is a hallmark symptom of EV-D68. This is often accompanied by sore throat and irritation.
-
Body aches: General muscle and body aches, similar to what one might experience with the flu, often occur alongside other respiratory symptoms.
-
Fever: Low-grade fevers are common in mild cases, typically resolving on their own within a few days.
-
Rash: Related to the coxsackievirus, many mpox patients have a pox-like rash appear on their face and body.
Severe Symptoms
-
Wheezing: One of the most concerning symptoms, especially in children with asthma. Wheezing occurs when the airways become constricted, making it difficult to breathe. For individuals with pre-existing respiratory conditions, this can escalate rapidly.
-
Difficulty breathing: Shortness of breath or labored breathing is a key indicator of severe EV-D68 infection. If untreated, this can lead to hospitalization and the need for respiratory support.
-
Paralysis: Although rare, EV-D68 has been linked to a condition called acute flaccid myelitis (AFM), which can cause sudden muscle weakness or paralysis, particularly in the arms and legs. This complication can develop days after the onset of respiratory symptoms and requires immediate medical attention.
The range of symptoms—especially the respiratory distress and potential for paralysis—makes early detection and appropriate testing critical. Individuals showing severe respiratory symptoms or those in high-risk groups should seek medical attention promptly.
If you think this virus sounds similar to COVID-19, you’re not alone. For more information on COVID-19, visit our website.
Is there a difference between rhinovirus and enterovirus?
Rhinovirus, a.k.a. the common cold, and enterovirus are both members of the Picornaviridae family but cause different illnesses. Rhinoviruses typically cause the common cold, while enteroviruses, including EV-D68, are linked to more severe respiratory conditions. To differentiate between the two, it’s important to test, especially when respiratory symptoms persist or worsen.
Why are Enterovirus tests relevant and important?
During outbreaks, early and accurate testing helps differentiate enteroviruses from other respiratory viruses like rhinovirus, flu, or RSV.
Testing is particularly important for high-risk individuals, such as children with asthma, to prevent complications. Understanding the strain responsible for an infection can guide treatment plans and public health interventions, especially during a widespread outbreak.
When to perform an Enterovirus test
Severe symptoms, such as wheezing or respiratory distress, warrant immediate testing. Enterovirus testing can also help rule out other viruses and assist in appropriate treatment planning.
Doctors note that children with asthma or other breathing problems are more likely to develop serious symptoms, and that wheezing coupled with traditional cold and flu symptoms is cause for concern. Whether you’re a parent, a physician, or both, if a child or patient has expressed any difficulty breathing or is wheezing, along with other symptoms of respiratory illness, it’s a good idea to have them tested for enterovirus D68.
3 types of Enterovirus tests available
There are three common types of enterovirus test that healthcare providers use to figure out what virus a patient has.
These tests include:
-
Polymerase Chain Reaction (PCR): This is the gold standard for enterovirus testing, as it allows for accurate detection and typing of the virus.
-
Virus Culture: This method involves growing the virus in a lab from the collected sample.
-
Microneutralization Test: Measures antibodies to detect exposure to enteroviruses.
In severe cases, spinal fluid tests, X-rays, blood tests, or ECG/Echocardiograms may be necessary to assess the full scope of illness.
Challenges associated with Enterovirus testing
Testing for enteroviruses can be complex due to the limited availability of specific typing tests in some healthcare facilities.
Additionally, distinguishing between enteroviruses and other respiratory illnesses such as rhinovirus or the flu can be difficult, which is why PCR testing is essential for accurate diagnosis.
Educating patients and parents about enterovirus tests
As a healthcare professional, it's important to reassure patients and parents that most cases of enterovirus, including EV-D68, are mild. Prevention through good hygiene practices, such as regular handwashing, is key.
Additionally, reminding parents that flu vaccinations can also help reduce the risk of severe respiratory illness will help combat the spread of this disease, especially during peak seasonal illness time.
How to perform an Enterovirus test
Accurate specimen collection is critical for diagnosing Enterovirus, and healthcare professionals must ensure they follow the right steps to collect samples efficiently and safely. Testing is typically conducted using real-time or nested PCR testing, which is performed by the healthcare professionals. The type of specimen collected—nasopharyngeal (NP) swabs, oropharyngeal (OP) swabs, stool samples, rectal swabs, blood, or cerebrospinal fluid—depends on the patient’s symptoms.
Step 1: Choose the right specimen based on symptoms
-
Respiratory Symptoms (cough, wheezing, difficulty breathing) warrant a nasopharyngeal (NP) and oropharyngeal (OP) swabs – a.k.a. a throat culture – are the preferred specimen types for detecting respiratory infections like EV-D68.
-
Gastrointestinal symptoms require a stool sample and rectal swabs may be collected.
-
Other complicated symptoms may lead to collection of blood and cerebrospinal fluid in more severe cases, especially if neurological symptoms such as paralysis are present.
For the sake of this step-by-step guide, we are going to assume that you will be collecting an NP or OP swab, as this is the most common.
Step 2: Collect NP and/or OP swab specimens
NP swabs are one of the most effective ways to collect respiratory samples. Follow these steps carefully to ensure accurate results:
-
Prepare for collection:
-
Wash your hands thoroughly.
-
Wear gloves, a surgical mask, and protective eyewear to prevent contamination.
-
-
Select the proper swab:
-
Choose a swab with a flexible plastic handle and a flocked tip, such as Puritan’s 25-3317-U, which is ideal for specimen collection in the nasopharynx.
-
-
Collect the sample:
-
Tilt the patient's head back slightly.
-
Insert the swab into one nostril, advancing straight back (not upwards) to reach the nasopharynx.
-
Rotate the swab up to 5 times and hold it in place for 5-10 seconds to collect sufficient material.
-
-
Store the sample:
-
Remove the swab and place it into a vial containing 1-3ml of viral transport media (such as Puritan’s UniTranz-RT™ system).
-
Break the swab handle at the scored breakpoint line.
-
Ensure the vial is properly labeled with the patient’s information (name, date of birth, and collection date).
-
-
Prepare for transport:
-
Secure the vial, ensuring the cap is tightened.
-
Deliver the sample to the lab for testing as soon as possible.
-
If an NP swab is not an option, or if an additional specimen is required, healthcare providers can perform an OP swab. This method is often used to sample the back of the throat and tonsillar area.
-
Prepare for collection:
-
Wash your hands thoroughly and wear protective gloves, a surgical mask, and eyewear.
-
-
Prepare the patient:
-
Ensure the patient is seated comfortably and facing a strong light source.
-
Ask the patient to tilt their head back, open their mouth wide, and stick out their tongue.
-
Use a wooden tongue depressor to keep the tongue in place and ensure visibility.
-
-
Choose the correct swab:
-
Use a sterile flocked swab, such as Puritan’s HydraFlock® swab, which is designed for optimal collection from the posterior nasopharynx and tonsillar arches.
-
-
Collect the Sample:
-
Without touching the sides of the mouth, carefully swab the back of the throat and tonsillar arches with the HydraFlock® swab.
-
Be sure to swab vigorously to gather enough specimen for testing.
-
-
Store the sample:
-
Insert the swab into a sterile liquid amies transport system vial, ensuring proper contact between the swab and the medium.
-
Break the swab handle at the scored breakpoint line.
-
-
Prepare for transport:
-
Secure the vial cap and ensure the sample is properly labeled with patient information (name, date of birth, collection date).
-
Deliver the sample to the laboratory for testing.
-
Step 3: Properly submit Enterovirus test samples for PCR testing
Once the NP or OP swab specimen is collected, it must be prepared and sent for PCR testing, typically performed by state health departments or the CDC. Follow these guidelines for submission:
-
Freezing and storing the sample:
-
Freeze the specimen at -20°C or lower within an hour of collection.
-
Samples can be stored for up to 60 days when frozen. If freezing is not an option, refrigerate the sample at 2°C to 8°C for up to 7 days.
-
-
Shipping the sample:
-
Pack the sample on dry ice to ensure it remains frozen during transport.
-
Be sure to include CDC Form 50.34 along with the sample for proper identification and documentation.
-
-
Double-check labeling:
-
Ensure the sample container is clearly labeled with patient information, including name, date of birth, collection date, and collection site.
-
Testing plays a crucial role in diagnosing and managing outbreaks, especially in high-risk populations such as children with asthma or individuals experiencing severe respiratory symptoms, so this protocol should be handled with the utmost care.
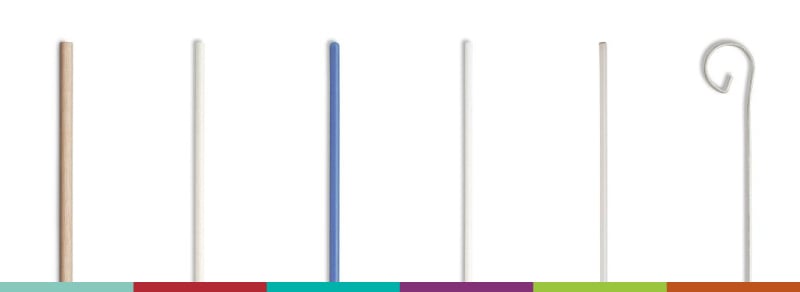
Puritan products to have on-hand to perform an Enterovirus test
Recommended Products:
UniTranz-RT™ Transport System: Ideal for the collection and transport of viral specimens, especially enteroviruses. Available with flocked or polyester swabs for optimal collection and transport.
One specific product example from this family of products is UniTranz-RT 3ml Filled Vial and 6" Sterile Ultrafine Flock Swab.
Additionally, flocked swabs, with the PurFlock Ultra 6" Sterile Ultrafine Flock Swab w/Polystyrene Handle, 100mm Breakpoint as a prime example, are perfect for enterovirus testing, as the collection and release properties of these swabs are superior to those of other collection swabs.
PurFlock Ultra 6" Sterile Ultrafine Flock Swab w/Polystyrene Handle, 100mm Breakpoint
Stock up your healthcare practice with the necessary swabs
Accurate enterovirus testing is essential for diagnosing and managing outbreaks, especially in vulnerable populations like children with asthma. By employing the proper testing techniques and specimen collection tools, healthcare providers can help control the spread of enteroviruses and ensure patients receive the care they need.
Ready to order?
Get in touch with one of Puritan’s customer support specialists and we’ll get you stocked up on the supplies you need so you’re ready to test for enterovirus.