When it comes to sexual health, early detection and treatment of sexually transmitted infections (STIs) are crucial for preventing the spread of infections. Among the various methods of STI testing, oral STI testing is an essential tool that ensures comprehensive care.
But what are the best practices around oral STI testing?
This guide aims to provide details on procedures and best practices for conducting oral STI tests, including tests for oral gonorrhea and chlamydia. We’ll also showcase which tools (swabs) healthcare professionals will want on hand to provide the best possible care to your patients.
Understanding Oral STIs
Oral STIs are infections that are non-genital—that is, they affect the mouth, throat, or tonsils—and are typically transmitted through oral sex. Common types of oral STIs include gonorrhea, chlamydia, herpes simplex virus (HSV), and human papillomavirus (HPV).
These infections can cause symptoms such as sore throat, ulcers, or lesions in the mouth, but they can also be asymptomatic, making regular testing essential for detection and prevention.
Importance of Oral STI Testing
Oral STI testing is crucial for several reasons, including:
Early detection and treatment
Identifying infections early allows for prompt treatment, reducing the risk of complications and transmission.
Preventing spread
Regular testing helps prevent the spread of STIs to sexual partners.
Protecting overall health
Untreated STIs can lead to severe health issues, including infertility and increased risk of HIV transmission.
“Regular STI testing is vital for maintaining sexual health and preventing the spread of infections. Many STIs can be asymptomatic, meaning individuals may not realize they are infected. Routine testing allows for early detection and treatment, reducing the risk of serious health complications and limiting transmission to others. It's a proactive step towards safeguarding both individual and public health.” - Virginia Templet, Puritan Medical Products
Types of Oral STIs and Testing Methods
Curious about the various types of oral STIs that healthcare providers test for? Here are the common ones:
Oral Gonorrhea
Oral gonorrhea can cause sore throat, swollen glands, and tonsillitis. If untreated, it can lead to more severe infections.
Oral Chlamydia
Oral chlamydia may cause sore throat, oral ulcers, and swollen lymph nodes. Untreated chlamydia can lead to severe reproductive health issues.
Oral Herpes Simplex Virus (HSV)
Oral swabs can detect HSV-1 and HSV-2, which cause oral and genital herpes.
Oral Human Papillomavirus (HPV)
Oral swabs can help identify HPV strains that may cause oral cancers.
For Healthcare Providers: How to Perform an Oral Swab STD Test
To accurately diagnose oral STIs, pharyngeal swabbing is the preferred method. This involves collecting specimens from the area behind the nasal cavities, mouth, and larynx. Here is a quick refresher if it’s been a little while since you’ve performed an oral swab for STIs on your patient:
-
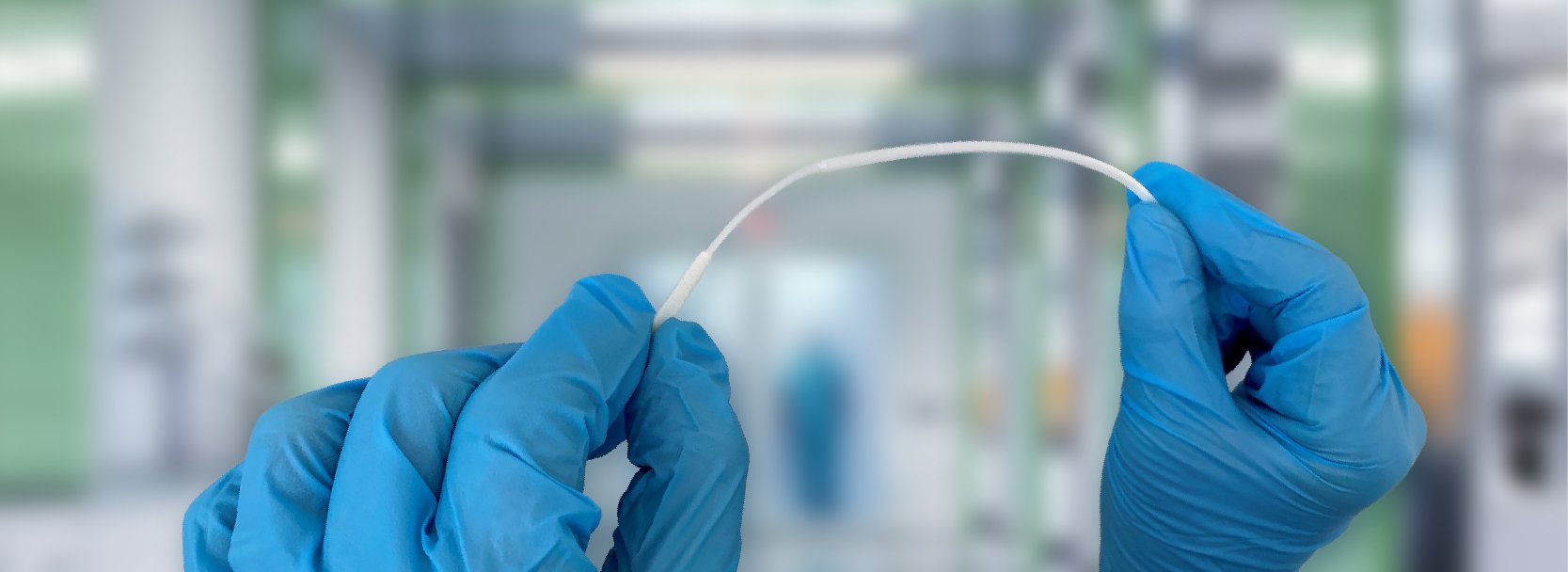
Step 1 – Preparation: Use a sterile flocked swab, ideally one that comes with a vial filled with transport medium, such as the Universal Transport Media system.
-
Step 2 - Patient Positioning: Instruct the patient to tilt their head back, open their mouth wide, and stick out their tongue.
-
Step 3 - Swab Collection: Carefully swab the posterior nasopharynx and the tonsillar arches without touching the sides of the mouth to avoid contamination. Ensure firm and thorough contact with the targeted areas to collect an adequate sample.
-
Step 4 - Sample Handling: Insert the swab into the vial containing 1-3 ml of transport medium immediately after collection. Break the swab handle at the scored breakpoint line to fit the swab securely into the vial.
-
Step 5 - Labeling: Label the vial with the patient’s information, including name, date of birth, and the date and time of collection, to ensure proper identification and traceability.
If you are looking for guidance on rectal or genital swabbing for Gonnorhea or Chlamydia, check out our helpful blog post that covers it all.
Best Practices for Accurate Oral STI Testing
To ensure the reliability of test results, healthcare providers should adhere to the following best practices:
Ensuring sample integrity
Use sterile, high-quality swabs specifically designed for microbiological sample collection. Flocked swabs, which have a brush-like tip, are particularly effective as they provide better sample retention and release.
Proper Collection Techniques
Follow precise collection protocols to ensure the integrity of the sample. This includes swabbing the correct anatomical sites thoroughly and consistently.
Immediate Transfer
Transfer the collected sample into the transport medium immediately to preserve the specimen's integrity and prevent degradation.
Accurate Labeling
Clearly label each sample with the patient's name, date of birth, and the date and time of collection. This is essential for maintaining traceability and ensuring that the results are correctly attributed to the right patient.
Detailed Documentation
Record additional details such as the type of test being conducted, the anatomical site of sample collection, and any relevant patient information. Proper documentation aids in maintaining comprehensive records and facilitates follow-up actions.
Avoid Contamination
Employ aseptic techniques during sample collection to prevent contamination. This includes using gloves, avoiding contact with non-sterile surfaces, and ensuring that the swab does not touch anything other than the intended collection site.
Provide Comprehensive Training
Ensure that all healthcare providers involved in sample collection are thoroughly trained in the correct techniques and procedures. This training should cover the entire process, from patient preparation to sample handling.
Adherence to Guidelines
Follow established guidelines and protocols set forth by health authorities such as the CDC or other relevant bodies. These guidelines are designed to standardize procedures and ensure the highest level of accuracy in testing.
Continual Education
Engage in continual education and training to stay updated with the latest advancements in STI testing and sample collection techniques. Regular training sessions and workshops can help reinforce best practices.
Appropriate Storage
Store collected samples at the recommended temperature to maintain their viability. For example, some samples may need to be refrigerated if not immediately processed.
Secure Transport
Use transport containers that protect the sample from extreme environmental conditions and physical damage. Ensure timely transport to the laboratory to prevent degradation.
Use Single-Use Instruments
Use single-use swabs and properly clean any re-used instruments that come into contact with the sample to eliminate the risk of cross-contamination between samples.
“Using the correct swab for oral STI testing is crucial for accurate results. High-quality, sterile swabs specifically designed for microbiological sample collection ensure optimal sample retention and release, which is essential for detecting infections. By choosing the right swab, we can improve diagnostic accuracy and provide patients with the most reliable results.” - Virginia Templet, Puritan Medical Products
Which leads us to…
We’re Here to Support You with Swabs for Your Patient’s Oral STI Test
Oral STI testing is a critical component of comprehensive sexual health care. By following the procedures and best practices outlined in this guide, healthcare providers can ensure accurate testing, early detection, and effective treatment of oral STIs. And to help, Puritan products are specifically designed for reliable sample collection and integrity
We recommend the following products for your oral STI swabbing needs:
- Polyester: 25-806 1PD, 25-806 1PD BT, 25-1000 PD
- Rayon: 25-806 1PR, 25-806 1PR BT, 25-800 R 50
- Flock: 25-3706-U, 25-3706-U BT, 25-3317-U, 25-3317-U
For high-quality swabs and testing products, contact Puritan Medical Products. Our knowledgeable product specialists are here to help!