In maternal health, knowledge is power – and when it comes to Group B Streptococcus (GBS), that knowledge can be a game-changer. The presence of GBS in expectant mothers is a significant concern in perinatal care. As healthcare providers, it's crucial to be well-versed in the implications, management, and testing protocols for GBS to safeguard maternal and neonatal health.
This blog post will serve as a refresher for swabbing for GBS and what tools are best for the job.
What is Group B Strep?
GBS, or Streptococcus agalactiae, is a type of naturally occurring bacteria found in the digestive tract of adults. GBS can pose a significant risk to newborns, pregnant women, the elderly and individuals with weakened immune systems. For the purposes of this blog post, we’ll be focusing on pregnant women and newborns.
GBS is primarily transmitted from mother to baby during childbirth, making it essential for pregnant women to be screened for GBS around the 35th to 37th week of pregnancy – in fact, one in four pregnant women are shown to have the bacteria. For context, in newborns, GBS infection can lead to serious health issues such as pneumonia, sepsis, and meningitis.
If identified, preventive measures such as administering antibiotics during labor can significantly reduce the risk of transmission to the infant. Timely diagnosis and management are crucial in preventing GBS-related complications, underscoring the importance of prenatal care and awareness about this bacterium in healthcare settings.
Group B Strep Swab vs 36 Week Swab: Is there a Difference?
They’re one in the same!
This is another term for a GBS screening test. Many people refer to GBS screenings as a 36-week swab because it’s a routine prenatal test performed between the 35th and 37th week of pregnancy.
Group B Strep – What to Watch Out For
GBS infections typically don't exhibit noticeable symptoms in healthy adults who carry the bacteria. However, when GBS causes infection, especially in the vulnerable populations we covered above, it can lead to a range of symptoms:
-
Newborns: GBS infection may manifest as fever, difficulty feeding, irritability and potentially life-threatening issues like pneumonia or sepsis.
-
Pregnant women: GBS infections might present symptoms like urinary tract infections (UTIs), high fever, chills and abdominal pain.
It's crucial to seek prompt medical attention if you or your baby display any concerning symptoms, particularly during pregnancy or shortly after childbirth. Early diagnosis and treatment are key to managing GBS infections effectively.
Why is a GBS Swab Important?
A GBS swab is crucial for several reasons. First, it helps prevent neonatal infections, as Group B Streptococcus (GBS) can cause severe conditions in newborns, including pneumonia, meningitis, and sepsis. Early detection through the 36-week swab allows healthcare providers to implement preventive measures during delivery to protect the baby.
Additionally, if the test results are positive for GBS, the mother receives intravenous antibiotics during labor, significantly reducing the risk of the baby becoming infected. This proactive approach not only ensures the health of the newborn but also provides peace of mind to the mother by managing potential complications effectively.
Types of Group B Strep
There are three types of group B strep disease:
- Prenatal-onset GBS disease: before birth
- Early-onset GBS disease: birth through the first week of life
- Late-onset GBS disease: over one week of age through several months of age
Women who are screened and test positive for prenatal-onset GBS can receive IV antibiotics during labor and delivery to help prevent early-onset GBS disease. Timing is crucial because GBS bacteria act incredibly quickly and can cause a healthy-seeming baby to fall critically ill.
Unfortunately, late-onset GBS disease can not be prevented, so it's best to test early. Group B Strep International advises that women have their first culture taken for GBS and other bacteria at least eight weeks after their last missed period.
Refresher: Collection of a Group B Streptococcus Swab Test
The American College of Obstetricians and Gynecologists recommends GBS screening between 36 and 37 weeks of gestation. Adequate training in the collection process is essential; the swab must be correctly inserted to obtain a representative sample. Strict adherence to aseptic techniques will minimize the risk of contamination.
It’s also vital to ensure that the culture is transported and processed under conditions that preserve bacterial viability. Providers should maintain open communication with their laboratory services to confirm timely and accurate assay interpretation. By rigorously following these procedures, healthcare providers can significantly reduce the risk of GBS transmission and its subsequent complications in newborns.
Can Women Collect a Self-GBS-Swab?
It’s not recommended.
While self-swabbing has become increasingly popular for its convenience and non-invasiveness, particularly in the context of sexually transmitted infection (STI) screening, it is not the recommended approach for GBS screening in pregnant women. The accuracy of GBS screening is paramount, as false negatives can lead to severe, life-threatening infections in newborns. Self-swabbing introduces a higher risk of improper sample collection and potential contamination, which can affect the sensitivity and specificity of the test.
Unlike STI screening, where self-swabbing may be comparably effective to clinician-collected samples, the complexities of GBS colonization and the critical need for precise diagnosis to inform the administration of intrapartum antibiotics demand a professionally executed procedure. It is essential that GBS cultures are collected by trained medical personnel to ensure the validity of the results and the safety of both mother and child.
Please see a trusted healthcare professional if you need to undergo GBS screening.
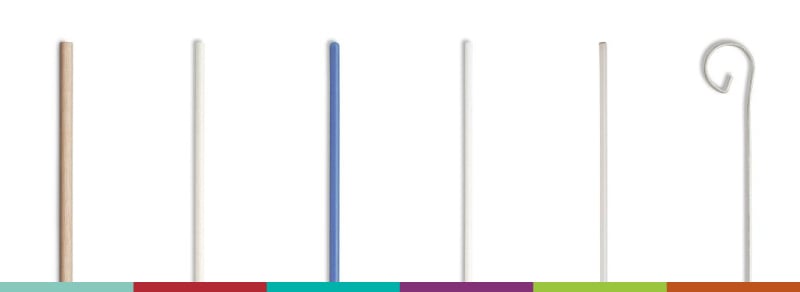
A Comprehensive Overview of GBS Swab Types
When collecting samples for GBS testing, selecting the right swab is critical for success. Several types of swabs are available, each designed to cater to different needs and environments. To start, we'll discuss the swabs used for GBS testing and the tip materials that make them the swabs of choice.
Here’s an in-depth look at the various types of swabs and their associated materials used in GBS testing:
Flocked Swabs
Puritan's HydraFlock® flocked swabs turn many short strands of fiber into a velvet-like brush – perfect for such an important task. Compared to conventional tip materials, the greater surface area of these many flock fibers results in superior collection and release of the specimen, and improved sensitivity of diagnostics tests. The increased number of target cells (compared to non-flocked swabs) help to improve the sensitivity of diagnostic tests. And our Lim Broth enrichment medium, which we created for use in the qualitative procedures for the isolation of GBS from clinical specimens, can help sustain the viability of the sample in settings where immediate laboratory processing is not possible.
However, if you want to explore other types of swabs, here’s the low down.
Foam Swabs
Puritan’s foam swabs are constructed with medical-grade foam that is soft and absorbent. They are suitable for collecting samples from sensitive areas without causing discomfort. The foam tip can hold and release the sample efficiently, making them a reliable choice for GBS testing.
Puritan 6 Inch Standard Foam Swab with Polystyrene Handle

Polyester Swabs
Puritan’s polyester swabs are widely used in clinical settings due to their excellent recovery rates of microorganisms. They are non-toxic and non-inhibitory, ensuring that the collected sample remains viable for testing. These swabs are ideal for GBS testing as they can efficiently capture and release bacteria from the sample site.
Puritan 6 Inch Standard Polyester Swab with Polystyrene Handle

Rayon Swabs
Lastly, made from spun rayon, Puritan’s rayon swabs are soft and absorbent, making them suitable for sensitive areas. They are commonly used in medical applications, including GBS testing, due to their ability to effectively collect and release specimens.
Puritan 6 Inch Standard Rayon Swab with Polystyrene Handle

Still unsure which GBS swab to go with? No problem—we’re here to help.
Step-by-Step Guide on How to Choose the Right GBS Swab
By understanding the different types of swabs and their materials, healthcare providers can make informed decisions when selecting the right swab for GBS testing. Using the appropriate swab ensures accurate and reliable results, ultimately contributing to better maternal and neonatal health outcomes.
Here are a few steps to follow to narrow in on the right swab for your patient:
Step 1. Consider the Sample Type
For GBS testing, it is crucial to choose a swab that can efficiently collect and release bacterial samples. Flocked swabs, such as HydraFlock® and PurFlock Ultra®, are excellent choices due to their high sample collection and elution capacities.
Step 2. Assess the Collection Site
The swab material should be suitable for the collection site. Foam swabs are ideal for sensitive areas, while polyester and rayon swabs are effective for general use.
Step 3. Evaluate Diagnostic Requirement
The sensitivity and specificity of the diagnostic test can be influenced by the swab type. Flocked swabs are known for their superior performance in diagnostic testing, making them a preferred choice for GBS testing.
Puritan is Here for GBS Swab Support
Have more questions about taking swab samples for group B strep, or about any of Puritan’s disposable medical products? Contact us to speak with one of our sales representatives.